News & Publications
Diagnostic Value of Preparing Cell Blocks from Pap Specimens
August 22, 2011
By Felix Martinez Jr, M.D.
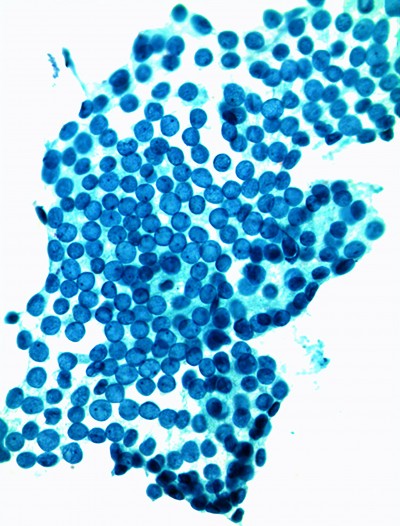
One interesting sidelight to the widespread use of liquid-based cytology (LBC) testing has been the development of a technique of preparing cell blocks from the fluid used for the detection and diagnosis of cervical lesions by Pap testing. Cell block preparation is useful for the detection and diagnosis of many other lesions, so why not use it as a complement to the Pap test, especially for diagnostically difficult cases?
Cell block preparation is a long established complementary method for examining nongynecologic specimens submitted to the laboratory. Cell block preparations have been used routinely for pleural fluid, peritoneal fluid, bronchial washings, fine-needle aspirations, and other cytologic specimens. Even after careful smear preparations, there often remains material in the specimen vial that would otherwise receive no further examination.
In cases in which few LSIL cells are present, using the cell block can improve the chances of identifying a lesion.
Although not needed in the majority of Pap tests, the addition of a cell block preparation can increase the sensitivity of detecting malignancies and has the ability to reduce false positive interpretations in selected cases.
Rarely, malignant cells not present on smears can be found in the cell block. In cervical collections, cases that are suspicious on smear might be diagnosed definitively with the aid of a cell block, illustrating that, sometimes, the best cytologic evaluation combines the use of both smears and cell blocks.
Histologic processing and sectioning of a cell block often enhances architectural features, such as gland formation, and highlights the relations between cytologically distinct cell populations. It also provides the opportunity to perform ancillary studies such as histochemical stains, immunohistochemical stains, and in-situ hybridization. In cases in which the specimen is clotted or is collected inadvertently into formalin -or in cases in which another handling or transport mishap has occurred- the cell block can provide an alternative means for evaluating material found unsuitable for direct smears.
Low-grade squamous intraepithelial lesions (LSIL) are usually fairly easy to find on a smear and are relatively easy to diagnose in a smear or monolayer. There are cases, however, in which the abnormal cells are in a “thick” group, or where they demonstrate an unusual
presentation, both instances where cell block preparation can assist in the diagnosis. In cases in which few abnormal cells are present, using a cell block can improve the chances of identifying a lesion, both because the cell block yields more cells to visualize and provides a different view of them.
The detection of high-grade lesions is the main concern in cytology screening. Abnormal cells in smears can be relatively easy to detect with both smears and cell blocks. Cells appear singly or in groups. Smears with large clusters or true tissue fragments of abnormal cells -often collected by overly vigorous brushing- are sometimes better visualized using the cell block technique. Characterization of some lesions that may be difficult to assess on smears is often enhanced by histologic sectioning.
The major disadvantages of adding a cell block to a gynecologic cytology case are the increased processing cost and lengthened specimen turnaround time.
Examples of difficult morphologic diagnoses include differentiating atypical immature squamous metaplasia from high-grade dysplasia, reactive endocervical cells from glandular dysplasia, and squamous from glandular differentiation in high-grade lesions. Samples with few abnormal cells or those with single cells that are small and are difficult to evaluate on thin-layer preparations and cell block. Examining a cell block along with a smear yields two differing, complementary views of the same cell population. We have found that this often increases specificity and/or reduces false-positive results.
The major disadvantages of adding a cell block to a gynecologic cytology case are the increased preparation costs and lengthened specimen turnaround time. Overnight tissue processing means that the case might not be reported until at least the next day.
With the advent of liquid-based Pap collections, the opportunity for cell block preparation is now available within the gynecologic cytology lab because a residual specimen is almost always present. In some difficult cases, p16 and Ki-67 immunostaining performed on cell block material can help distinguish neoplastic from low grade or nonneoplastic lesions.
For more information, please contact one of Incyte Diagnostic’s Board Certified pathologists.