News & Publications
Should Oral HPV Testing Be Performed to Screen for Oral Carcinoma?
June 1, 2013
The number of HPV-related oropharyngeal carcinomas is on the rise according to the Annual Report to the Nation on the Status of Cancer, 1975-2009; however, we still don’t have an accepted screening protocol in place to address the situation. The U.S. Preventive Services Task Force states that it is difficult to detect oral cancer and that the evidence is not clear whether oral cancer screening improves long-term health outcomes among the general adult population or among high-risk groups.
More high-quality research is needed on whether screening tests can accurately detect oral cancer and if screening adults for oral cancer in primary care settings improves health outcomes. The ADA Council on Scientific Affairs believes that further research is required to improve the understanding of the natural history of oral HPV infection, transmission risks, screening, testing, and the predictive value of a positive HPV test for the subsequent development of oropharyngeal cancer.
The behavior of cervical cancer is similar to oropharyngeal cancer, with persistent viral infection causing genetic changes then cell transformation. In addition, oral HPV infections can be either low-risk types that do not cause cancer or high-risk types that can cause oropharyngeal cancer. In contrast to cervical cancer, there is no accepted screening shown to reduce incidence or death from oropharyngeal cancer. There is no approved diagnostic work-up and treatment regimen for oropharyngeal cancer that will prolong disease-free survival and reduce cancer specific mortality.
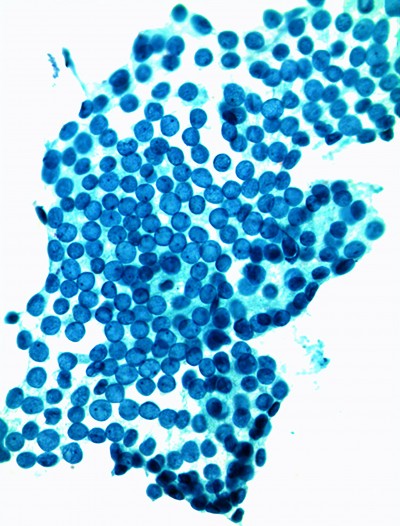
One reason is that screening is problematic. There is no proven Pap-like test that collects cells with a cytology brush for screening and early detection of HPV-associated oropharyngeal cancer with acceptable sensitivity and specificity. Cytologic evaluation of the oropharyngeal region is useful in detecting invasive oropharyngeal cancer, but has limited utility as a screening modality for populations without visible lesions or clinical disease. Many HPV related oral cancers develop deep within the folds of the tonsils so the developing cancer cannot be seen and is not readily accessible for brush sampling.
In 2007, the World Health Organization said there was sufficient evidence to conclude that HPV16 was the cause of oropharyngeal cancer and people with HPV16 oral infection are at a 15-fold higher risk for oropharyngeal cancer and a 50-fold increased risk for HPV-positive head and neck cancer. However, the detection of cancer is only the first step in a screening process. With cervical HPV, if there were cytologic abnormalities, patients were referred for a colposcopy and biopsy. A similar treatment algorithm does not exist for oropharyngeal cancer.
Until the natural history of oral HPV infection is better understood, the utility of identifying populations at a high risk of oropharyngeal cancer through detection of oral HPV infection is unclear. The absolute risk of oropharyngeal cancer among individuals with oral HPV infection is unknown. As data is collected, HPV vaccines may eventually prevent these cancers by helping people avoid initial infection by immunity.