If you have any additional questions regarding your bill, please feel free to call one of our knowledgeable billing specialists at 509.509.4519.
1. Can I set up a payment plan?
Yes. You can set up a payment plan in our online portal or call our business office and set one up over the phone. We are happy to work with all of our patients.
2. Can I pay with a credit/debit card?
Yes, we accept Visa, MasterCard or Discover. There is no additional charge for this service. Click here to pay your bill online.
3. Can I pay with a check?
Yes, you can pay with a check by phone, online, or by mail.
4. Where did you get my personal information such as insurance carrier, personal address, phone number, etc.?
Your information is submitted when your specimen is sent here for processing by the clinic/physician’s office/hospital.
5. Who are you?
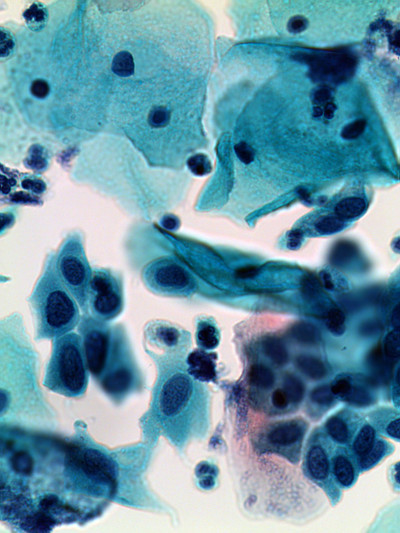
Our group of pathologists serves communities in Washington, Idaho, Oregon, Montana and Alaska. Our physicians, board certified in the specialty of pathology, provide professional laboratory support to health care providers for hospitals and physician offices and clinics. Our pathologists evaluate Pap tests, molecular lab tests and biopsy (surgical) specimens to diagnose your condition to help your attending health care providers determine the best treatment option(s) for you.
6. What is this bill for?
A tissue, cellular collection, or body fluid obtained at either a doctor’s office or hospital and labeled with your name was submitted to our laboratory. Our pathologists are the specialists who evaluate the pathology specimen and provide diagnostic information to your doctor as to whether the sample contained any abnormalities.
7. Why do I have two bills? One from Incyte Diagnostics (Pathology) and one from the hospital?
In these cases, the hospital has provided the technical portion (TC) or preparation of your specimen, and they are billing you for those services. Incyte Diagnostics has provided the professional portion (PC) or the actual interpretation and reporting of your specimen by a pathologist. An explanation of this is also found on the back of your Incyte statement.
8. What is an “EOB”?
EOB stands for Explanation of Benefits. The medical insurance company sends the patient and the provider a form summarizing the insurance plan’s coverage for a specific medical event (procedure, test or supplies), including the amount that needs to be paid by our patient.
9. Did you / Why didn’t you bill my insurance?
If your insurance was billed, it would be noted on your statement from us. You may call to confirm this using the phone numbers listed on your statement.
If your insurance was not billed, there are several explanations why you might receive a bill even though you have medical coverage:
- Perhaps our billing department did not receive the complete insurance information or patient details for us to submit a claim
- A call to your insurance may also provide a more complete explanation of your policy benefits.
- Sometimes the insurance carrier has been billed, but the payment was denied. If a denial is the cause of your receiving a bill from Incyte Diagnostics, please refer to the EOB (Explanation of Benefits) mailed by your insurance company. The EOB form states the reason(s) for denial.
- If you are a Medicare patient, it is possible that you will be responsible for charges if the service is defined by Medicare as a non-covered charge, or you have agreed to pay for services by signing an Advanced Beneficiary Notice (ABN) before the specimen was collected. Many oral or dental biopsies are not covered by Medicare, instead they are often considered a dental procedure and therefore are not covered.
- If you wish to submit billing information directly, please contact our Billing Department.
To view a list of current insurance contracts, please click here.
10. What does “deductible” mean?
The deductible is the amount of money in the insurance company's plan year that the patient must pay before the insurance will start paying. The amount varies according to the contractual terms of the individual insurance policy.
11. When are tests or screenings considered not preventive?
Your preventive benefits offer full coverage for many tests, screenings and immunizations. During your preventive exam, your doctor may find an issue or problem that requires further testing or screening for a proper diagnosis to be made. Also, if you have a chronic disease, your doctor may check your condition with tests. These types of screenings and tests help to diagnose or monitor your illness. These diagnostic tests are not covered by your preventive benefits and often require you to pay a greater share of the costs. For example, a routine colonoscopy may be covered under preventative benefits but once a polyp is found, the biopsy is NOT typically covered under preventative benefits and therefore is subject to deductibles and coinsurance. A biopsy cannot be billed with routine codes.
Premera/Bluecross patients please see https://www.premera.com/documents/022325.pdf
Medicare patients please see http://www.medicare.gov/coverage/colorectal-cancer-screenings.html
12. How can I obtain the results of my biopsy/Pap tests?
The best place to obtain your results is through the physician that sent the specimen to Incyte Diagnostics. A report has been sent to them with the results of the testing. It's always best to get results from the clinician who is treating you.